WHAT IS THE CORNEA?
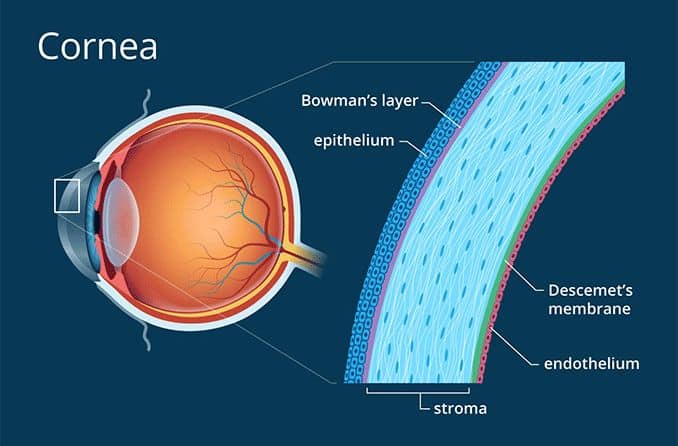
The cornea is a clear layer that covers the front of the eye. It helps the eye focus and keeps out germs and dust. Corneal diseases include infections, degeneration of the cornea and inherited conditions.
BLEPHARITIS
Blepharitis is chronic redness and irritation of the eyelids.
Blepharitis cannot be cured, but it can be controlled with a few simple, daily hygienic measures, such as the following:
- At least twice a day, place a warm, wet washcloth over your closed eyelids for a minute. Rewet it as it cools, two or three times. This will soften and loosen scales and debris. More important, it helps liquefy the oily secretions from the eyelids’ oil glands, which helps prevent the development of a chalazion, an inflamed lump in an eyelid oil gland.
- With your finger covered with a thin, wet washcloth, cotton swab, or commercial lint-free pad, gently scrub the base of the lashes for about 15 seconds per lid. You can use baby shampoo diluted in water to scrub which can help remove debris and crusting
When medications are necessary, they may include:
- artificial tears (over-the-counter eyedrops) to relieve symptoms of dry eye;
- antibiotics (oral or topical) to decrease bacteria on the eyelids; and
- steroids (short-term), to decrease inflammation.
Medications alone are not sufficient to control blepharitis; the application of warmth and detailed cleansing of the lashes daily is the key.
KERATOCONUS

Keratoconus is an uncommon condition in which the dome-shaped cornea (the clear front window of the eye) becomes thin and develops a cone-like bulge. As the condition progresses, the shape of the cornea is altered, distorting your vision. Usually, keratoconus affects both eyes, although symptoms and progression in each eye may differ.
Early symptoms include mild blurring of vision, increased sensitivity to light and glare, and mild eye irritation. The rate of progression varies. Keratoconus usually begins in the teenage years. It may progress slowly for 10 to 20 years and then suddenly stop. As it progresses, the most common symptoms are increased blurring, increased nearsightedness or astigmatism, inability to wear contact lenses, and frequent eyeglass prescription changes.
The causes of keratoconus are not known. Since an estimated 10% of people with keratoconus have a family member with the condition, some researchers believe genetics may play a role.
Keratoconus is usually corrected with eyeglasses. However, as the condition progresses, rigid contact lenses may be needed so that vision is improved. If vision is greatly affected, a corneal transplant may be recommended. While this procedure will relieve the symptoms of keratoconus, it will not cure it completely. Nonetheless, in advanced keratoconus corneal transplants offer the best prognosis for clear vision.
A new treatment called collagen cross-linking recently has been evaluated in the treatment of progressive keratoconus and has been shown to be effective in some patients. The provincial government funded a study (2012-2015) and is still reviewing the results to determine whether the procedure will be funded under OHIP. For now it is an uninsured service though you may be eligible for treatment at no cost at academic vision centres in Ontario. Check with your ophthalmologist to see if you are a good candidate.
CONJUNCTIVITIS

“Pink eye,” the common name for conjunctivitis, is an inflammation or infection of the conjunctiva. The conjunctiva is the outer, normally clear covering of the sclera (the white part of the eye). The eye appears pink when you have conjunctivitis because the blood vessels of the conjunctiva are dilated. Pink eye is often accompanied by a discharge, but vision is usually normal and discomfort is mild.
Either a bacterial or a viral infection may cause conjunctivitis. Viral conjunctivitis is much more common. It may last several weeks and is frequently accompanied by a respiratory infection (or cold). Antibiotic drops or ointments usually do not help, but symptomatic treatment such as cool compresses or over-the-counter decongestant eyedrops can be used while the infection runs it course. The virus that causes COVID-19 can cause conjunctivitis and be transmitted to others. Unlike viral conjunctivitis, bacterial conjunctivitis can be treated with a variety of antibiotic eyedrops or ointments, which usually cure the infection in a day or two.
Conjunctivitis can be very contagious. People who have it should not share towels or pillowcases and should wash their hands frequently. They may need to stay home from school or work, and they should stay out of swimming pools.
Not all cases of conjunctivitis are caused by an infection. Allergies can cause conjunctivitis, too. Typically, people with allergic conjunctivitis have itchy eyes, especially in spring and fall. Eyedrops to control itching are used to treat allergic conjunctivitis. It is important not to use medications that contain steroids (names of steroids usually end in “-one” or “-dex”) unless prescribed by an ophthalmologist.
Finally, not all cases of pink eye are caused by conjunctivitis. Sometimes more serious conditions, such as infections, damage to the cornea, very severe glaucoma, or inflammation inside the eye will cause the conjunctiva to become inflamed and pink. Vision is usually normal when pink eye is caused by conjunctivitis. If your vision is affected or you experience eye pain, it is recommended that you see an ophthalmologist.
